Living with Psoriasis and Psoriatic Arthritis
One thing a lot of people don’t know about me is that I’ve been living with two autoimmune disorders for almost ½ of my life.
Psoriasis and Psoriatic Arthritis.
Like all chronic diseases there are significant challenges involved with managing my health so I decided to share my journey in hopes that it might help someone going through a similar journey, but also to educate others on two diseases that millions of Americans suffer from.
In future blogs I will also discuss how I am using a Ketogenic lifestyle to keep down inflamation in my body and live a healthy live with a diet full of fats and void of carbs:) But first I thought I should start with some background on what I've been through to get to this point.
I will warn you that this is a long post, but I couldn't think of any ways to share this story without just getting it all out at once! I hope I can find some people who can relate to this journey, and maybe even my learnings will help someone else!
First you might be wondering "What is Psoriasis and Psoriatic Arthritis?"
PSORIASIS 101
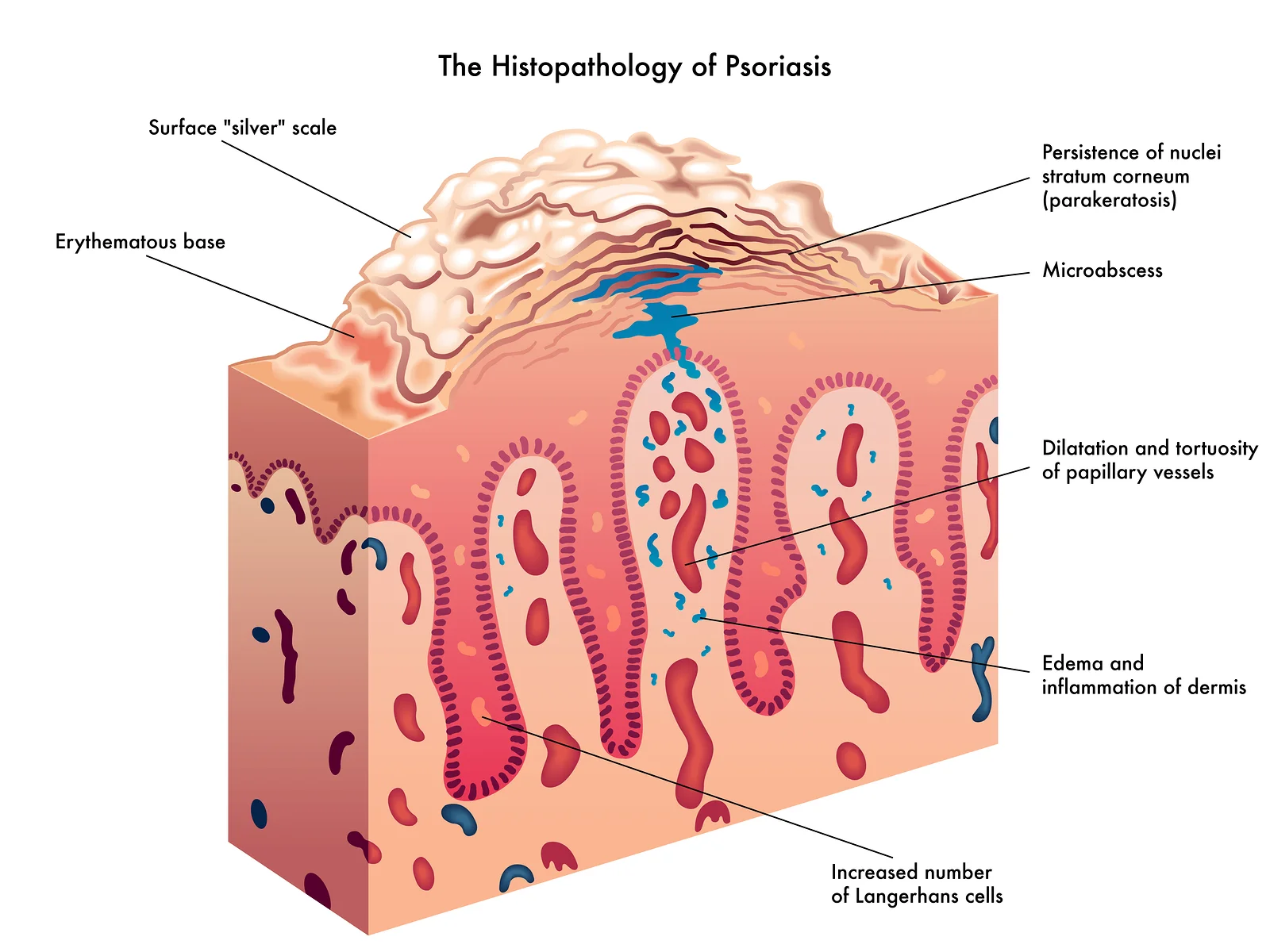
The science of Psoriasis
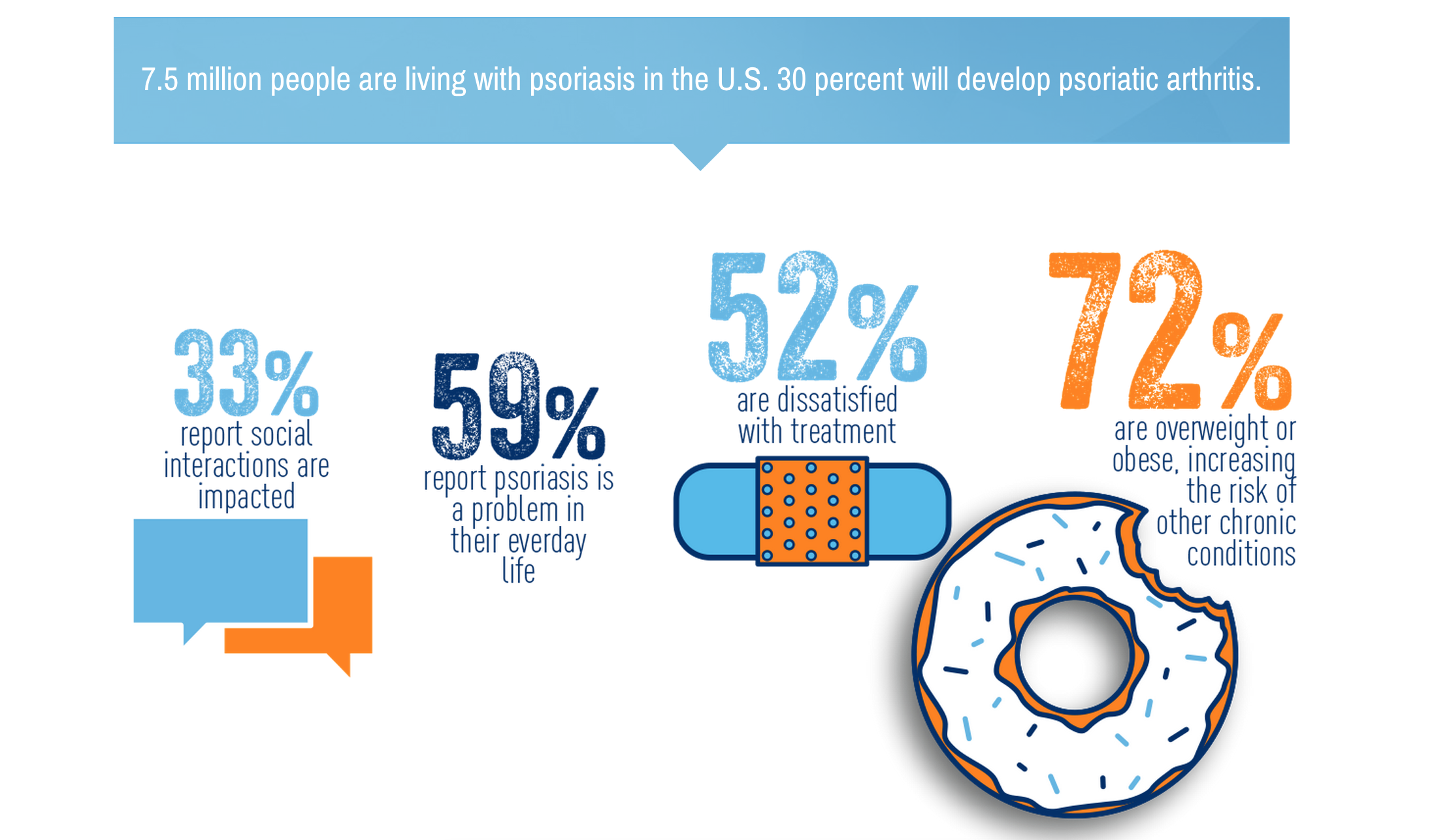
A lot of people think Psoriasis is a skin condition, like eczema. But in fact, while it displays itself on the surface of the skin in the form of red patches, the problem starts deep inside the immune system. People with Psoriasis have overactive immune systems, causing new skin cells to be produced every 3 to 4 days instead of the typical 28 to 30. 7.5 million Americans suffer from Psoriasis.
Eczema by contrast usually occurs because of a hypersensitivity reaction to some sort of irritant (perfumes, dyes, animals etc…). This causes an itchy red rash that 30 million Americans get, luckily many of them grow out of it as they get older.
Psoriasis however, is forever. To determine if you have Psoriasis you need to see a Dermatologist. Finding a Dermatologist that specializes in Psoriasis isn't necessarily difficult, but it does require asking the right questions. There are plenty of Derms out there who seem to be more interested in Botox these days than helping people with an autoimmune disorder like Psoriasis. Ask the receptionist if there is anyone in the office that specializes in Psoriasis, do your research online, visit forums.
Doctors can test for Psoriasis by doing a skin biopsy where they take a chunk of skin about the size of a pencil eraser to be tested. They have done this a couple times to me and I have the scars to prove it:) They also may just look at the skin as well as the fingernails which are often affected.
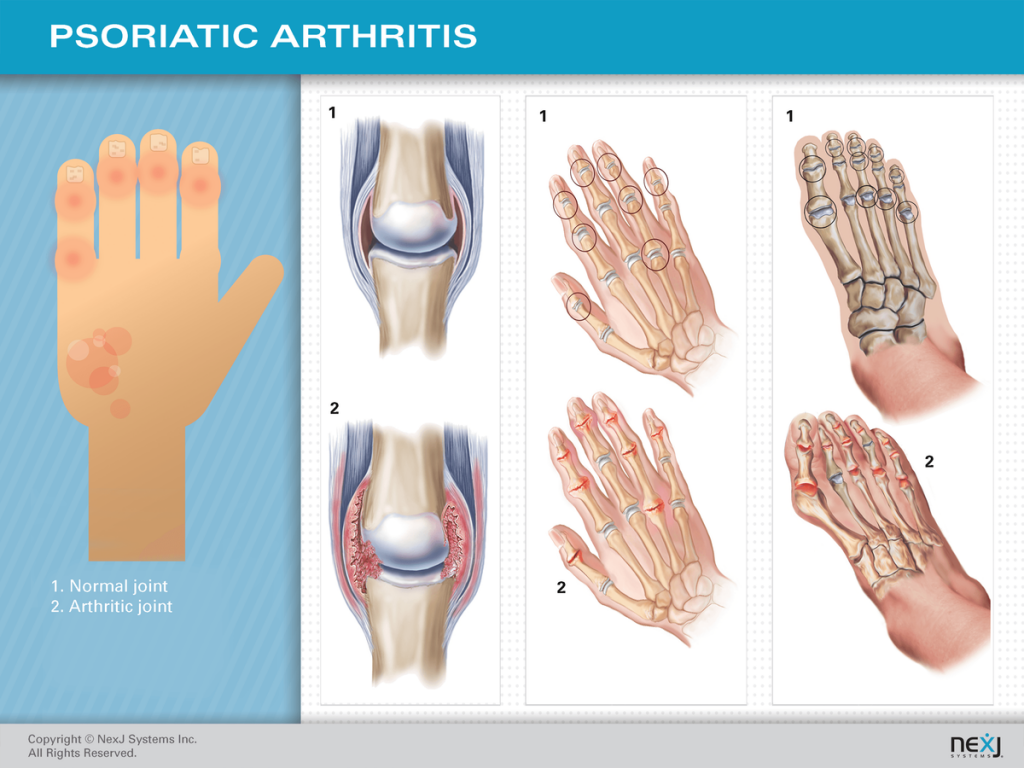
PSORIATIC ARTHRITIS 101
Psoriatic Arthritis involves joint pain, stiffness and swelling. It can affect any part of the body, but common areas include feet, hands and spine. Common symptoms include fatigue, tenderness over tendons, swollen fingers and toes that look like sausages, reduced range of motion, and pitted nails.
There is no test for Psoriatic Arthritis, the diagnosis is made through a series of observations, X-rays, and other tests by a Rheumatologist. It is extremely important to get diagnosed early because joint deformity can happen quickly, but studies estimate that as many as 1 in 4 people diagnosed with Psoriasis may have undiagnosed Psoriatic Arthritis.
HOW I FOUND OUT
My journey with Psoriasis started when I was 18 and living in the dorms. At first it was just a couple small spots, but I instantly knew what they were because my Dad has struggled with the disease since he was in his late twenties. What I didn’t realize at this time was how much more challenging the disease would be for me as a woman of “child-bearing age” which is a term I started hearing over and over again throughout my years of treatment.
6 months after I found my first Psoriasis spots I discovered I also had Psoriatic Arthritis. The arthritis did not tip-toe into my life. It made itself known with one huge kick in the ass! I was home for the summer from college, woke up one day and from what I can remember could not move my muscles. None of them.
I felt stiff as a board. I had no idea what was going on. I had always been an athlete, I was in great shape from being a competitive soccer player but all of a sudden I was 19 and I couldn’t get out of bed without my parents’ help.
My dad knew exactly what was happening, again because of his experience with the Psoriasis, and got me into a Rheumatologist that day. I did not know people with Psoriasis could also get a certain kind of arthritis at that point, but I was about to get my education. The doctor felt my joints and instantly told me I had Psoriatic Arthritis.
Up to 30% of people with Psoriasis can develop Psoriatic Arthritis, most don’t develop the two one right after another like I did. In fact my Dad, who is 64 has just in the last couple years started developing some Psoriatic Arthritis in his fingers some 35 years after developing the Psoriasis. But for me it pretty much all came at once.
Having Psoriasis alone makes you nearly twice as likely to develop an additional autoimmune disease*. But if you have both psoriasis and psoriatic arthritis, like I do, then your risk for an additional autoimmune increases even more. There is also an increased incidence for lymphoma, heart disease, depression and more. The emotional impact is substantial, in fact the prevalence of depression in patients with psoriasis may be as high as 50%. Studies have shown that Psoriasis patients experience mental and physical disability just like patients with other chronic illnesses such as cancer, hypertension, heart disease and diabetes.
So yea, it can be a lot to take in. I’m 37 now, and thankfully I have been very healthy for the last 4-5 years. But my twenties and early thirties were a complete roller coaster so I wanted to share some of those moments with everyone.
EARLY 20s
During this period of my life I was getting used to the idea that this was going to stick around forever. Like most women I want to feel beautiful and wear whatever I want. But that can be hard to do when you are covered in red patches. So that was a struggle.
The reality is, for me at least, that these 2 diseases require some pretty major medications to even keep it in check. Since they are caused by an overactive immune system I need to be on medications that suppress my immune system which in turn slows the damage done to my joints. In my 20s my Doctors put me on a combination of topical ointments, biologic medications, and a nasty medication called Methotrexate.
The ointments were expensive and messy. They usually would give you one tiny tube that was supposed to last the whole month and it would last me like 3 days when my flare ups were really bad because I would need to put it on my whole body. Plus at this time I wasn’t making a lot of money so half the time I didn’t want to spend my last $60 on some tube of ointment. I remember I would try to get all of the samples I could from the Doctors. I would also buy anything I saw at the drugstore that said it would help psoriasis. Most of that stuff does not work, the one thing that does is also the grossest, smelliest treatment of all - coal tar treatments. I don’t have one in particular I would recommend because it has been so long since I have used any, but they do provide relief if you don’t mind smelling like a freshly paved driveway and staining every set of sheets you have!
The biologics were really new when I first got the diseases. I was usually one of the first to try any of them because the way it works is they get approved first for Rheumatoid Arthritis (I assume because more people have that which equals more $$$$ for the companies) and then once that happens they get around to approving it for Psoriatic Arthritis years later. So my Doctors would fight with the insurance companies until they approved me and luckily they always did!
On the topic of insurance, let me just mention really quickly that I have been lucky enough to have a very stable career, starting at age 21, so I have always had solid PPO health insurance. I know a lot of people are not as fortunate which is heart breaking. These medications, the biologics especially are EXPENSIVE! So that has been key. I honestly don’t know how anyone could manage this disease without great health insurance. So if you have a condition like mine and your work gives you options of HMO or PPO I would say it is worth the money to go for PPO- you need to be able to be in control with diseases like this. Ok, back to the drugs...
Enbrel was the first biologic drug approved for RA. It was approved for Rheumatoid Arthritis by the FDA in 1998 which is the year I got diagnosed, so I guess you could say if you were going to get Psoriatic Arthritis I picked a good time haha. Enbrel is a shot you inject into yourself like most of the other biologics. It may sound familiar these days because pro Golfer Phil Mickelson has Psoriatic Arthritis and now does their commercials.
They would always pair the biologics with Methotrexate. Methotrexate is awful. It looks harmless because it is just tiny little pills which you take once a week in whatever quantity prescribed (which later I would take as an injection) but it made me feel so sick. They use it for cancer patients and it can also damage your liver. I think it was more mental than anything but every time I would take it I would gag because I felt like I was poisoning myself. In fact I Googled it to include an image here and literally the gagging feeling came right back to me and put a weird taste in my mouth.
This treatment plan would work really well for awhile, during that time period I would often go into denial that I had the disease at all because I would feel normal. But like any autoimmune disease, they don’t stay away for long. My body seemed to have a cycle, and that cycle meant that after 18 months the biologics would stop working because my body would build up an immunity. So then we would need to try something else.
Luckily new drugs were coming out during this time, so there was something new to try. The bad part is that it takes awhile to get these medications approved by insurance, and then once they do it takes a good 3-4 months for them to start working (or to even tell if they will work at all!). So that meant periods of 6 months or more where I was not doing very well so I compare these years to a roller coaster because I was either feeling almost normal or completely awful- not much in between.
AGE 25
This was a very eventful year- I got pregnant! Luckily I had not been taking my Methotrexate for a few months before that, not because I was planning it but because I was a being a bad patient (ha!). I was just so over it all at that point. I was on a biologic at the time, I honestly can’t remember if it was Humira or Enbrel (because I have taken both at one time or another) but I stopped taking it when I found out I was pregnant. (Note: some people do take these medications throughout pregnancy without issue, there is a lot of info online. But over 11 years ago when I was pregnant there was not much info because the medications were super new, so I opted to not take anything.)
The doctors said my Psoriasis would probably be ok during my pregnancy without the medication because apparently many women have that reaction to the hormones. That was not the case for me. My skin was covered in painful psoriasis the whole second half of my pregnancy. There were plenty of days I just couldn’t function my skin hurt so bad. My arthritis however was somewhat under control until I gave birth and then all hell broke loose.
I gave birth to my daughter Kaia in May of 2004 when I was 26. She was totally healthy and was born right on her due date which I appreciated:) I nursed her for about 6 weeks until I couldn’t handle the pain of the 2 autoimmune issues and then got back on a biologic medication, this time Remicade.
It took awhile for the Remicade to start working, it can take 3 months or so to start kicking in. Even then it doesn’t just magically make everything better, it takes a long time to get the joints and then the skin under control again.
During this time I also did phototherapy light treatments which helped my skin. Throughout the years I have also spent a fair amount of time in tanning beds because they do help me. I always say I have to "pray the skin gods won’t give me skin cancer because they have already given me enough to deal with"!
LATE 20s
After having a baby I did have joint deformity happen in my left ring finger as a result of being off of my medications for an extended period of time. You can see my pinky and middle finger have now joined the party too, although not as extreme as my ring finger. But it was a small price to pay for my Kaia Bear who is now 11. And now that I am divorced I like to say it is my reminder to not get married again;)
The Remicade worked well for me in my mid to late twenties and it was definitely my favorite biologic because instead of having to give myself a shot you go into the Doctors office and get an IV for two hours every 6-8 weeks. Much easier and it worked for awhile, about two years I think.
But by now you are noticing a trend- the meds stop working eventually. This is around the time I started experimenting with some alternative therapies including going to a chiropractor and trying acupuncture. I didn’t really notice an improvement from either. However, my acupuncture Dr (he was an actual MD) told me I should cut sugar out of my diet all together because the inflammation that sugar causes was making my skin and joints worse. I did it and he was right! Diet made a huge difference, especially in my skin. The psoriasis was much less angry looking and I continue eating this way today 95% of the time (with a few lapses here and there).
To this day almost none of the Doctors I have seen give any credit to diet at all. I think it’s crazy that they can’t recognize how the food you put into your body can effect what is happening inside your body, but most have no interest in hearing about it (in my experience).
30s
When I was 30 my daughter and I moved to Santa Fe, New Mexico for a new job opportunity. This meant all new Doctors, which would become an issue. In addition to a Dermatologist and Rheumatologist, I also started visiting an allergy specialist in Santa Fe. The concept of the treatment was that they would identify what you are allergic to, put you on a strict diet without those items and then would inject you in small doses with the allergens so that eventually you would not be allergic to them anymore. It’s called LDA or Low Dose Allergen therapy. The Doctor had worked with patients with RA and other autoimmune disorders and was confident it would work, so I had hope. I was also pretty desperate for something to work long term. I had felt some promise from the success of the low sugar diet and hoped this would be equally successful. lt was expensive because the doctor didn’t take insurance, but I was willing to try anything. I was also on traditional medications at this time (same old cocktail of Topical Ointments + Methotexate + Biologic). I continued down this path for about a year and then one day something went very wrong.
It started in my ankle. It got very swollen and sore. I went to urgent care, they sent me to the emergency room because they thought I was septic. The emergency Doctors said I was not septic, they said it was Cellulitis and put me on some antibiotics.
Over the next week my body started really freaking out. I was at work and my vision went blurry, my face got really hot and my skin turned red from head to toe. I went to the allergen doctor I had been seeing and gave me a Kenalog shot, 100,000u of Vitamin D, Prednisone, Borage Oil, Fish Oil and Zinc and got me an appointment with an Internal Medicine Doctor he knew.
I remember it was Halloween time because we had to go to a Halloween festival at Kaia’s school so I came up with a costume that covered every square inch of my body and put so much makeup on to cover the red and then just prayed no one would notice. When you have a condition like Psoriasis it is so hard to hide, you just start hoping no one looks at you at all. I look pretty normal when you see these pretty pictures, but they don’t tell the real story...
My ankle was feeling better thanks to antibiotics and from first glance I look like I am feeling great but underneath I looked like this...
This turned into about a month of going from Doctor to Doctor trying to figure out why this happened. Was it the combo of the Allergen treatment and the antibiotics? Or the antibiotics and the biologics? No one knew.
One Doctor thought I had Steven Johnson Syndrome, 2 thought I also had Lupus. The tests all came back inconclusive. I wasn’t getting any answers, but every day I got worse and worse.
There I was in New Mexico, with no friends, no family, just Kaia and I. It was a definite low point for me. I couldn’t even get in my car without crying because of the combination of joint pain and skin pain. One big lesson I learned was that I should have been going to doctors at a University Teaching Facility from the start.
When I lived in Denver I did go to a teaching hospital, University of Colorado, and now that I live in Los Angeles go to UCLA. But in New Mexico I had been going to local doctors in Santa Fe. The problem with that is that if something goes really wrong, like it did for me, it takes a long time for the doctors at the teaching hospitals to see you. Even if other doctors call on your behalf, like they did for me. I ended up finally got into the University of New Mexico Dermatology department on November 24, so about 5 weeks after this journey began.
I had to take Short Term Disability from work during this time because all of my time was spent going back and forth to Doctors appointments trying to figure out what was going on with my body, plus I was in no condition to work and looked rather frightening.
Right after Thanksgiving I tried to go back to work and this included a leadership meeting in Denver for 5 days. By Friday I was counting down the minutes until the meetings were over and as soon as they were I realized I needed to go to the hospital. I think I took a cab, I walked into the emergency room the receptionist took one look at me and said “come with me”. I looked that horrible. They didn’t ask me any questions, they didn’t have me fill out any forms, they just led me straight to a room.
Me looking terrifying as I was admitted to the hospital.
I wondered after this all happened how on earth my coworkers stared at me for 4 days in a tiny conference room and didn’t tell me to get my butt to the hospital sooner. I ended up having to stay at the hospital for 7 nights.
They tested everything, took skin biopsies to make sure I really had Psoriasis (I did- I could have told them that), and gave me lots of drugs, LOTS. Btw Morphine mixed with Benadryl is a CRAZY combination!
The best part about being in the hospital was that I could focus 100% on my health. I had an unlimited supply of ointment for my skin which was in terrible shape- 85% of my body was covered in psoriasis I estimate, maybe even more. The Doctors and nurses had never seen anything like my skin apparently, there were basically tours that would come through looking at me (the downside to a teaching hospital), but they were very kind.
On my 6th day in the hospital they put me back on Remicade with the hopes that my body wouldn’t have the tolerance built up anymore and then I went back to New Mexico. This is what my skin looked like when I left the hospital. I could only stand for short amounts of time because every inch of my skin was very painful, even the bottom of my feet.
My welcome home present from Kaia, a stuffed animal Christmas tree. You can see how red my face and hand was even in this lo-res photo.
Then it was time to go back home to Santa Fe to see my daughter and rest. A week or so later we flew to New York to spend Christmas at my parents’ house. My skin was still very painful at this point, I was putting on ointment multiple times a day, taking oatmeal baths, sleeping with plastic wrap around my body to seal in the ointments- I was a mess. I was also taking a new medicine for me called Soriatane. I had tried to get on this medication for years, but because I was of “child-bearing age” they wouldn’t give it to me.
I remember how much it hurt to put those tights on that night. It took me like 30 minutes just to put those on. But I was determined to look good for Christmas.
The reason for that is because Soriatane can cause birth defects in babies- it is from the Accutane family. So I had to ensure the Doctors I did not want anymore children before they would put me on it. Before this drama I had multiple Doctors tell me I would have to have a hysterectomy before they would prescribe it for me. Finally after all of this drama they put me on it.
I was also on a lot of Prednisone steroids at this time and had been since the “freak out” first started. My doctors in New Mexico had started stepping me off of them, but apparently not slow enough. The day before Christmas my hair started falling out in big clumps and by January 20th it was 90% of my hair.
WIGGIN' OUT
When I went back to work I did so with a wig. I ordered a couple online because I was too embarrassed to go to the wig store with my psoriasis covered skin and scalp. One thing I remember very clearly during this time period was the shame I felt about my skin and my condition. People are really very rude about skin conditions in general. People would stare or tell me how “red I looked” all the time. “Were you brunt?” they would say. “Can I catch it?” they would say. Little kids not knowing any better would point it out all the time.
I was turned away more than once from getting a massage. One time a woman wouldn’t cut my hair. It was humiliating. I hope people reading this who do not have Psoriasis or any other sort of skin condition will realize that it is not appropriate stare at someone or ask them unsolicited questions. Again, I really just wanted to disappear. I certainly did not want to engage in conversation with total strangers about my health issues.
So anyway… the wigs. I tried to make the most of it. I would get a new one every month or so. Different colors, always the same style. My thought process was maybe people would just notice the color and not that it was a wig. I’m sure people noticed but no one pointed it out.
I would love to say I got home from the hospital, got lots of rest over the holidays, threw on a wig and was healed- but that isn't what happened. My skin continued on this roller coaster in January, February, March, and April. I honestly don't remember how my joints were doing at the time. The hard part is that some treatments that might make your arthritis better can aggravate your skin or vice versa so it was a frustrating few months with the joints and the skin. So even though I was on Remicade during this time period (having started it in December in the hospital) it still hadn’t really kicked in.
I had become a pro at this point in dressing in things that totally cover me. It was like a game trying to figure out how to cover up and still look cute. I also became a pro at faking like I felt ok. I would still try to rally to go out with my friends, I would still go on dates, I just tried to be as normal as possible.
May 2011
Eventually the Remicade and other meds started working and slowly but surely my skin started clearing up and I started feeling good again. From the day that ankle started swelling to the moment I felt better was about 7 months. In May of 2011 I felt much better. You can see me here in the pool with my wig on but with my skin looking clear (bright red, but clear). Then once Kaia was done with her school year I decided it was time for us to get out of New Mexico. Within a 2 week time period I found an apartment on the beach in Marina Del Rey, CA, we packed up our belongings and landed on the sand!
Moving to California was the best decision I ever made. First of all I am obsessed with the ocean, so it just put me in a calmer place immediately. Secondly I had a good network of friends in LA, so it automatically felt more like home from the day we arrived.
After a year and a half in a wig I had enough hair for extensions. My best friend in Colorado, Jamie Staton, owns a salon so I flew out to see her to get my extensions. Her cousin Lisa is their extension wizard so she and Jamie collaborated on a highlight, Brazilian Blowout and Extension overhaul that had me feeling like my old self again. I am so grateful to them for doing that for me, it was a huge turning point for me. I felt normal again!
After an afternoon at Salon Cosabella I looked like my old self again!
After 10 months of extensions I took them out once my real hair had a chance to grow. It came back curly!!! Never in my life have I had curly hair, but my “new hair” was totally different. Now that it is longer, it pretty much just has a few random kinks in it vs actual curls but I’m still amazed at how different the texture and everything is.
One very important lesson I learned is to be very, very careful if I ever go on Prednisone again. Doctors are very quick to prescribe it and I understand that it is needed sometimes, but if you are ever on a large dose for an extended period of time, like I was, then you need to be extremely careful in how they step you down otherwise you could end up bald like me!
TODAY (2015)
It was a long road, but now it has been 5 years and I am still on Remicade. In fact today as I am writing this it is December 9th, 2015. I received that first IV of Remicade in the hospital in Denver on December 9th, 2010.
I have felt great for the last 4 ½ years (my dosage has been doubled since then but is still working for now). I went off of Soriatane once my skin was clear, as an experiment with my Dr to see if the Remicade could keep it clear. That was a few years ago and it’s still clear. My joints are doing pretty well too. There is definitely permanent damage to my joints, but the biologics are slowing down that process. I never went back on Methotrexate, they want me to but I just won’t at this point.
I have had two surgeries on my left ring finger to try to straighten it back out, the most recent one was in 2015, but no luck. The joint is gone so will need replacing at some point but because I’m still young they don’t want to do it yet.
UPDATE (2018)
It’s been a few years since I added to this post, so I wanted to let you know how my treatments have been going. In January 2016 I started the ketogenic diet to try and help manage the inflammation in my body and my autoimmune disorders. I started having stomach issues in 2015 and went through a lot of testing, as Drs thought I might have Crohn’s Disease. Once you have an autoimmune disorder it is easier to “collect” others. But I decided to turn to food to see if I could help myself out. I went gluten free first and within a week I noticed an improvement. I did that for 6 months and then decided to take it further and started looking into low carb approaches again. I had done Atkins before, but wanted to see what else was out there. I read the Bulletproof book and Grain Brain and also did some research online, which is how I learned about keto. It sounded like something I could do, so I started on January 6th, 2016.
2 years and almost 10 months later I can confidently say keto is now just my way of life. I can’t imagine ever going back to eating a traditional diet. It keeps me feeling satisfied, I have lost 40lbs, the inflammation in my gut is healed, and I feel like I am doing everything I can to keep my body in a place where it can focus on healing.
Does that mean I have cured my Psoriasis and Psoriatic Arthritis?
NO. Not even a little.
Keto is not going to cure the destruction of my joints, which even with the strongest meds available is happening at what I find to be an alarming rate. Not everyone with PsA will have this experience, but I have a very destructive form of PsA. About 6 months ago the Remicade that had worked so well for me for 7 years stopped working. It was very difficult for me to accept because I had felt so good, and nothing had ever worked that long. But it got to a point where 2 weeks after an infusion my joints would hurt again (infusions were happening every 6 weeks), so I knew I had no choice but to switch to something else.
In the last 6 months I have tried a few combinations, so far nothing has worked great. I tried Cosentyx but it did not work for me. My Psoriasis has broken out again and my joints have been sore. Mainly my hands, feet and knee are affected right now in terms of joints. My current medications are Xeljanz and Methotrexate. They tried Arava first instead of MTX because of my hatred for MTX, but it didn’t work so MTX was my only option. I have a better attitude about Methotrexate this time around though because it really is my only option as a companion drug, so I just need to suck it up. I’m 3 weeks into a larger dose of it and I do think I am starting to see improvement. Within 4-8 weeks you can usually tell if it is going to work and 3-6 months should show maximum effectiveness. So I have a little ways to go, but I feel hopeful. I take the Zeljaz every day (it’s a pill) and I take 9 Methotrexate pills every Friday. The MTX pills wipe me out for at least a day, so Friday night is the perfect time to take them.
Currently I am only seeing a Rheumatologist, not a Dermatologist because in my experience once the joints start improving with meds the skin will follow. I did have my Rheumatologist prescribe me some basic topicals, but otherwise I am depending on the drugs.
I also had my first joint fusion in the last 6 months. My thumb joint (the middle joint, Metacarpophalangeal Joint or MP) on my right hand. The arthritis had destroyed the joint, so fusing it was the best option. Below are photos of my hand before the surgery and after. A nice big scar reminds me of it, but overall the healing hasn’t been so bad. I will need to do the same surgery on my left thumb eventually, but so far the joint is holding on a little while longer. I don’t have full motion, but I can do most things I could do before since my hands have already been limited by arthritis, this is not a big change for me.
So as you can see the journey never ends when it comes to autoimmune disorders. I firmly believe that Keto has been a powerful tool for me in managing inflammation. I do not just want to rely on drugs, even though I know that for me drugs are also a necessary part of my treatment. A keto lifestyle is not going to stop my joints from destructing, so I need the combination of both to optimize my health.
Hopefully sharing this crazy journey will help someone. Autoimmune disorders are connected to every part of your life because they are triggered by lack of sleep, stress, unhealthy lifestyle, and more. People assume since I have a suppressed immune system that I must get sick all the time, but I actually don’t! I do get plenty of sleep and stay pretty healthy. However, if I get off my schedule I can get run down pretty fast and if I do get sick, I have a harder time getting rid of it than most people so it’s important that I act quickly and get myself to a doctor even if it seems harmless at first.
2020 (UPDATE)
I’ve been on Xeljanz and Otezla all of 2019 and 2020 and it suddenly stopped working. So as of May 2020 I started Tremfya. I am documenting how it working for me in the links below. Tremfya is an injection I give myself. I take a loading dose at week 0 and week 4. Then I take one every 8 weeks after that.
WHAT DOESN’T KILL YOU MAKES YOU STRONGER
November 2015
I pray I don’t pass this onto my daughter because I know how hard it has been to deal with this when I was so young. But if she does, I will be well equipped to help her with the lessons I have learned from years of trial and error.
In the end it’s easy to say things like “what doesn’t kill you makes you stronger” but it has been hard to keep a positive attitude at times. I know the journey is never over, but I try to live in the moment and not worrying about what health challenges might lie ahead. It’s not worth the stress. I do my best to live a lifestyle that doesn’t put me at any additional risk. I get a good amount of sleep, I do follow a Ketogenic diet, and I am really good at relaxing on the weekends;)
I hope this starts an open dialogue for other people that are overcoming their autoimmune issues to live a positive, adventure filled life. I am proud to say I have not used my medical issues as an excuse to not live life to the fullest. I have an amazing daughter and family, a great group of friends, a really cool career, and the resources to take care of myself so I am absolutely grateful.
For anyone who would like more information on Psoriasis and Psoriatic Arthritis I would recommend www.psoriasis.org as a great resource. If you have additional questions you can email me at ketointhecity@gmail.com
xx
* A study published in November 2012 in the Journal of the American Academy of Dermatology